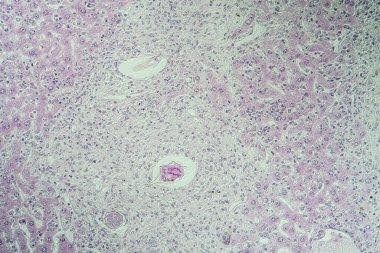
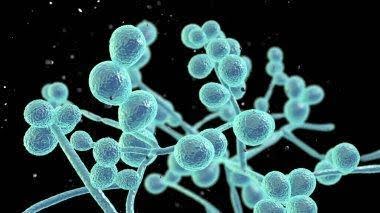
Candida is the name for a group of yeasts (yeast is a type of fungus) that commonly infect the skin. The name ‘candida’ refers to the white color of the organisms in culture. Candidal infection is known as ‘candidiasis’, ‘candidosis’ or ‘moniliasis’.


Candida depends on a living host for survival. It is a normal inhabitant of the human digestive tract from early infancy, where it lives without causing any disease most of the time. However, if the host’s defenses are lowered, the organism can cause infection of the mucosa (the lining of the mouth, anus and genitals), the skin, and rarely, deep-seated infection.
The most common Candida (C) species to result in candidiasis is C. albicans. Other non-albicans candida species are:
- tropicalis
- parapsilosis
- glabrata
- guilliermondii
Acute pseudomembranous candidiasis, also known as thrush, is the most common form of oral candidiasis, it is important to recognize that other types of oral candidiasis exist and that candidal infection can present as white and erythematous lesions. White lesions include acute pseudomembranous candidiasis and chronic hyperplastic candidiasis; red lesions include acute and chronic erythematous candidiasis, angular cheilitis, median rhomboid glossitis, and linear gingival erythema. Other rare oral types not included in these categories are cheilocandidiasis, chronic mucocutaneous candidiasis, and chronic multifocal candidiasis.
Types of Candidal Skin Infections
Oral Candidiasis (Oral Thrush)


Oral candidiasis is an infection of the oral cavity by Candida albicans. The condition is generally obtained secondary to immune suppression, which can be local or systemic, including extremes of age (newborns and elderly), immunocompromising diseases such as HIV/AIDS, and chronic systemic steroid and antibiotic use.
Risk factors for the pathological colonization of Candida include but are not limited to malnourishment, age extremes (young children and elderly), metabolic disease, immunocompromising conditions, concomitant infections, radiation therapy, organ transplantation, long-term steroid treatment, antibiotic treatment, and salivary gland hypofunction.
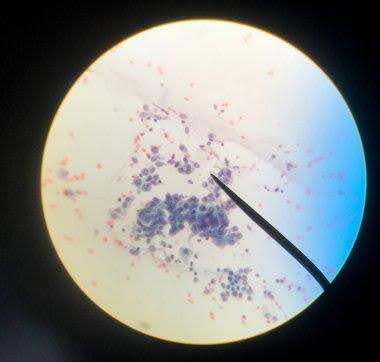
Diagnosis of oral candidiasis is often clinical, based on clinical examination, medical history taking, and assessment of risk factors. A biopsy is recommended for certain types in addition to empirical treatment. Cultures are usually done if antifungal treatment is ineffective. Topical antifungal therapy and oral hygiene measures are generally sufficient to resolve mild oral candidiasis, and systemic antifungal therapy is usually reserved for patients who are refractory or intolerant to topical treatment and those at increased risk of developing systemic infections.
Angular Cheilitis


Angular cheilitis is a common, non-contagious, inflammatory condition affecting the corners of the mouth or oral commissures. Depending on the underlying cause, it may last a few days or persist indefinitely. It is also called angular stomatitis, cheilosis, rhagades, or perleche (perlèche). Angular cheilitis occur at the angles of the mouth where two different types of skin lining meet and act as a hinge. The lining of the oral cavity (oral mucosa) meets with squamous epithelium (facial skin). As they are used often for eating, drinking, and talking, they are vulnerable to stress/trauma.
Angular cheilitis most commonly occurs due to prolonged exposure of the corners of the mouth to saliva and its digestive enzymes, resulting in eczematous cheilitis (a form of irritant contact dermatitis)
Symptoms include:
- Painful cracks/fissures worse on mouth opening, Blisters, erosions, oozing, crusting, Redness (or pallor/darkening of the skin in some cases), Bleeding.
- In many cases, no treatment is needed and angular cheilitis resolves by itself.
- General measures Include:
- Improved general hydration
- Use of lip balm or a thick emollient ointment applied frequently (often sufficient treatment alone for saliva-induced angular cheilitis)
- Topical antiseptics
- Specific measures
- Depending on the specific cause, oral and topical treatment options include:
- Topical antifungal cream
- Oral antifungal medication
- Topical or oral antistaphylococcal antibiotic
- Topical steroid ointment if the skin is significantly inflamed.
Vulvovaginal Candidiasis (Genital Infection in Women) including Cyclic Vulvovaginiti
Candida can cause an infection if conditions change inside the vagina to encourage its growth. Things like hormones, medicines, or changes in the immune system can make infection more likely. The common term for candidiasis in the vagina is a vaginal yeast infection. Other names for this infection are vaginal candidiasis, vulvovaginal candidiasis, or candidal vaginitis.
The symptoms of vaginal candidiasis include:
- Vaginal itching or soreness
- Pain during sexual intercourse
- Pain or discomfort when urinating
- Abnormal vaginal discharge
Vaginal candidiasis is often mild. However, some women can develop severe infections involving redness, swelling, and cracks in the wall of the vagina.
Vaginal candidiasis is common. Women who are more likely to get vaginal candidiasis include those who:
- Are pregnant
- Use hormonal contraceptives (for example, birth control pills)
- Have diabetes
- Have a weakened immune system (for example, due to HIV infection or medicines such as steroids and chemotherapy)
- Are taking or have recently taken antibiotics
Healthcare providers usually diagnose vaginal candidiasis by taking a small sample of vaginal discharge. They examine the sample under a microscope in the medical office or send it to a laboratory for a fungal culture. However, a positive fungal culture does not always mean that Candida is causing symptoms. Some women can have Candida in the vagina without having any symptoms.
If you have vaginal candidiasis, likely you will use anti-fungal medicine to treat it. Often, the treatment is an anti-fungal medicine applied inside the vagina or a single dose of fluconazole taken by mouth. You may need other treatments if your infection is more severe, doesn’t get better, Keeps coming back after getting better.
These treatments include:
- More doses of fluconazole taken by mouth
- Other medicines applied inside the vagina, such as boric acid, nystatin, or flucytosine
Balanitis (Penile Infection)


Balanitis is a treatable condition that most commonly happens in uncircumcised males. The main symptoms of balanitis include inflammation and pain on the head of your penis. Circumcision is a procedure that removes skin (the foreskin) from the head of the penis (glans). Yeast infections typically cause balanitis. However, bacterial infections, viral infections and some skin (dermatological) conditions can also cause balanitis.
Balanitis isn’t a sexually transmitted infection (STI), and it isn’t contagious. However, certain STIs may cause balanitis, and balanitis can look like an STI.
Symptoms include:
- Pain and irritation on the head of your penis
- Discoloration or discolored patches on your penis
- Itching under your foreskin
- Swelling
- Areas of shiny or white skin on your penis
- White discharge (smegma) under your foreskin
- A foul smell
- Pain while urinating (peeing)
- Sores or lesions on the head of your penis. (This symptom is rare and appears with PKMB, which affects people over 60.)
Untreated balanitis can cause chronic (long-term) inflammation. Lasting inflammation can lead to health issues, including Balanitis xerotica obliterans, Phimosis.
The treatment for balanitis depends on what’s causing the condition. Treatments can include:
- Antifungal creams
- Antibiotics
- Diabetes management
- Circumcision
Cutaneous Candidiasis


Candida infection of the skin is a yeast infection of the skin. The medical name of the condition is cutaneous candidiasis. Candida is the most common cause of diaper rash in infants. The fungi take advantage of the warm, moist conditions inside the diaper. Candida infection is also particularly common in people with diabetes and in those who are obese. Antibiotics, steroid therapy, and chemotherapy increase the risk of cutaneous candidiasis. Candida can also cause infections of the nails, edges of the nails.
Symptoms include:
- Red, growing skin rash
- Rash on the skin folds, genitals, middle of the body, buttocks, under the breasts, and other areas of skin
- Infection of the hair follicles
- Intense itching
It is more likely in the following circumstances:
- Infancy or old age
- Warm climate
- Occlusion eg, plastic pants (babies), nylon pantyhose (women), dental plates
- Broad-spectrum antibiotic treatment
- High-estrogen contraceptive pill or pregnancy
- Diabetes mellitus, Cushing syndrome and other endocrine conditions
- Iron deficiency
- General debility as from cancer or malnutrition
- Underlying skin disease as psoriasis, lichen planus
- Immunodeficiency as low levels of immunoglobulins, infection with human immunodeficiency virus (HIV)
- Chemotherapy or immunosuppressive medications including systemic steroids.
Treatment include:
Good general health and hygiene are very important for treating candida infections of the skin. Keeping the skin dry and exposed to air is helpful. Drying (absorbent) powders may help prevent fungal infections. Losing weight may help eliminate the problem if you are overweight. Proper blood sugar control may also be helpful to those with diabetes. Antifungal skin creams, ointments, or powders may be used to treat a yeast infection of the skin, mouth, or vagina. You may need to take antifungal medicine by mouth for severe candida infections in the mouth, throat, or vagina.
Invasive Candidiasis
Invasive candidiasis refers to spread of candida through the bloodstream (candidaemia) and infection of heart, brain, eyes, bones, and other tissues. This occurs in patients that are very unwell or that are immune suppressed. The common species of candida are usually found on culture, but sometimes one of about 15 other species are detected, such as:
- C. auris
- C. haemulonii
The most common symptoms of invasive candidiasis are fever and chills that don’t improve after antibiotic treatment for suspected bacterial infections.
People who are at high risk for developing invasive candidiasis include those who:
- Have spent a lot of time in the intensive care unit (ICU)
- Have a central venous catheter
- Have a weakened immune system (for example, people on cancer chemotherapy, people who have had an organ transplant, and people with low white blood cell counts)
- Have recently had surgery, especially multiple abdominal surgeries
- Have recently received lots of antibiotics in the hospital
- Receive total parenteral nutrition (food through a vein)
- Have kidney failure or are on hemodialysis
- Have diabetes
- Are pre-term babies
- People who inject drugs are also at risk for invasive candidiasis, especially for bloodstream infections, heart valve infections, and bone and joint infections.
Invasive candidiasis doesn’t spread directly from person to person. However, some species of the fungus that causes invasive candidiasis normally live on skin, so it’s possible that Candida can be passed from one person to another and possibly cause an infection in someone who is at high risk.
Prevention includes : Antifungal medication, hygiene.
Symptoms of a yeast infection may mimic other conditions. Hence physical examination and laboratory testing are very important. The risk factors that may increase the chances of developing a yeast infection include antibiotic usage, diabetes mellitus, pregnancy, hormonal birth control, and immunocompromised conditions such as HIV, chemotherapy, or some medications. It is essential to test and diagnose accurately when symptoms are bothersome and before starting any treatment.
Hygiene and effective treatment helps in getting relief from Candidiasis.
